Serena had been taking her antiretroviral drugs religiously for just over a year. She had fewer infections, gained weight and was feeling quite well. Then she visited the health clinic near her home and her physician sent her to the lab. Two weeks later, her community health worker brought her a message that she was to return to the clinic. When she saw the doctor, he told her that her viral load was increasing and he did not think her current antiretroviral (ARV) regimen was working — he would have to switch her to a new regimen and then re-check her viral load. Serena was glad they learned what was not working before she developed more symptoms.
Serena is not a real patient, but stories like this happen all over the world and demonstrate why viral load monitoring is the preferred approach to diagnosing treatment failure in people who are receiving antiretroviral treatment. The test gives patients a way to know if their drugs are effective at suppressing the virus and — if they are not — tells doctors they need to prescribe a different antiretroviral regimen that may be more effective for that patient.
As countries follow international best practices to treat and prevent the spread of HIV — and to meet their “third 90” target for the UNAIDS 90-90-90 strategy — successfully scaling up viral load monitoring is critical for progress. But for many countries, doing this with tight budgets and all of the logistics involved can be challenging. Therefore, effective laboratory supply chains play a critical role in ensuring that working instruments, and the right products, in the right quantities, are available throughout the laboratory system.
To support that goal, GHSC-PSM, PEPFAR and other U.S. government agencies are now prioritizing the implementation of an “enhanced network approach” to providing laboratory services for viral load monitoring.
The enhanced network approach is based on the realization that in many countries, simply providing testing equipment and supplies is not sufficient to increase use — stakeholders must also take into consideration the location and placement of that testing equipment within a given geographic region to optimize laboratory network performance and ensure those most in need of services — like viral load monitoring — can access them.
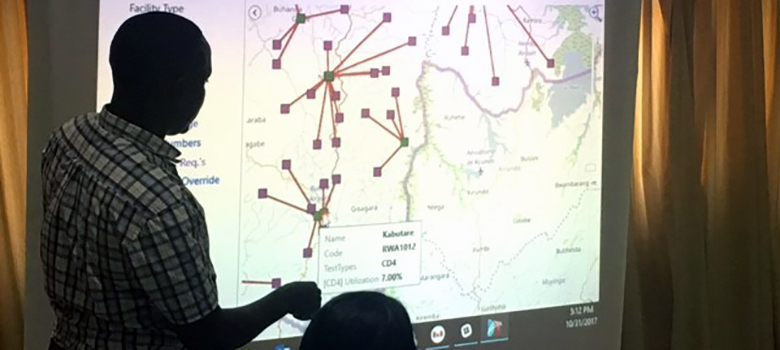
Towards these efforts, USAID is supporting the use of the Laboratory Efficiency and Quality Improvement Planning, or LabEQIP software tool. LabEQIP is an open source tool that can act as a data repository for information relevant to a laboratory network’s performance. It collects data and provides users with the ability to visualize lab network performance and available resources through an array of maps and charts. These visualizations then enable the user to make data driven informed decisions and assess the impacts of donor and stakeholder interventions over time.
In early November, GHSC-PSM and USAID supported a workshop in Entebbe, Uganda with the aim of orienting key partners to the use of LabEQIP and helping them to evaluate and optimize their laboratory networks, thereby supporting broader efforts to scale up viral load monitoring.
Participants from PEPFAR implementing partners, USAID, the CDC, and Ministries of Health from seven countries — Cameroon, Kenya, Malawi, Swaziland, Tanzania, Uganda and Zambia — attended the conference. Participants provided data prior to the workshop that they fed into LabEQIP — with trainer support — to learn how to use their own data to allocate resources, identify specific areas of improvement, and assess the appropriateness of the location of instruments within their own laboratory networks.
After the course, GHSC-PSM expects participants to use their new skills to inform national laboratory network strategy, share course materials with co-workers and work with their own laboratory managers to strategically plan improvements to their laboratory networks.