Assessing the benefits and risks of vaccination and communicating them widely to the public is essential to protecting public health and strengthening trust in vaccines. This was especially true with COVID-19 vaccines, which came to market rapidly due to the urgent need. Many potential vaccine recipients had concerns about the safety of the shots, partly because of the rapid speed at which they were developed. To get shots in arms, governments around the world aimed to assure the public that health agencies were taking the public’s concerns seriously through pharmacovigilance programs.
The Ethiopian Food and Drug Authority (EFDA) coordinates the country’s drug safety monitoring and reporting. At the regional level, regional health bureaus (RHBs) and woreda health offices (WoHOs) lend their help. However, considering the country’s total population, Ethiopia’s health facilities submit comparatively few reports about adverse events following immunization. Moreover, limited human resource capacity at all levels of the national pharmacovigilance system is a key reason for historically low numbers of investigations and assessments on serious adverse events. Inadequate collaboration among public health programs has also been a limiting factor.
With COVID-19 vaccines scheduled to arrive in 2021, the Ethiopian government mobilized relevant partners, including the USAID Global Health Supply Chain Program–Procurement and Supply Management (GHSC-PSM) project, to help gather information about the vaccines’ safety from vaccination sites across the country.
GHSC-PSM partnered with relevant government agencies, including the Ethiopian Food and Drug Administration (EFDA), RHBs, regional regulators, WoHOs, expanded program of immunization (EPI) units, and vaccination centers to help the country ensure the safe use of vaccines. This meant improving Ethiopia’s national and subnational pharmacovigilance capacity, including monitoring, detection, recording, reporting, investigation, and analysis.
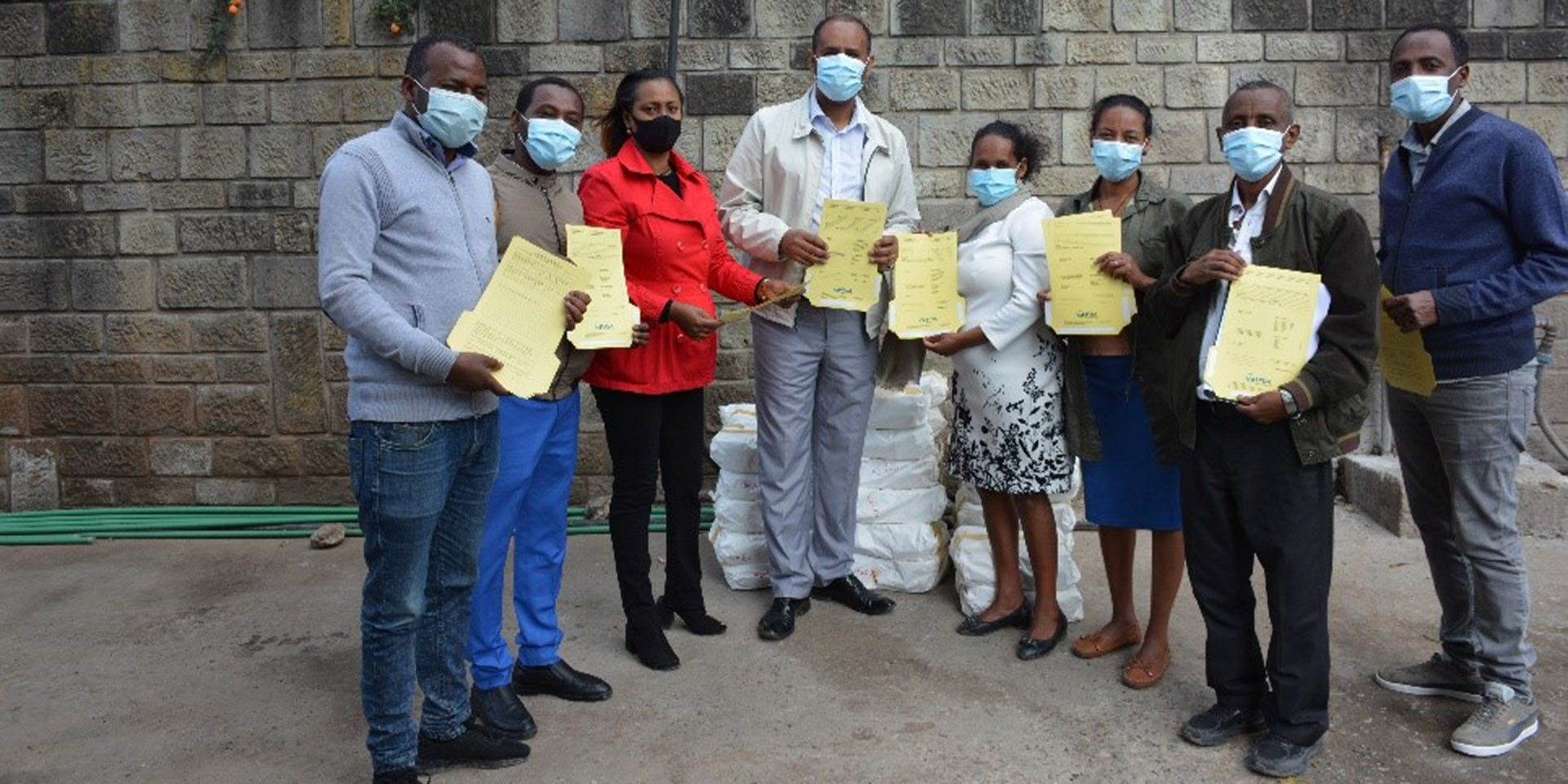
GHSC-PSM partners with these stakeholders to develop guidelines and training manuals, provided pharmacovigilance reporting tools, conducted training and orientations, and conducted supportive supervision at vaccination centers.
GHSC-PSM’s activities to support pharmacovigilance included:
- Developing risk management plan guidelines for market authorization holders, standard operating procedures for reporting adverse events, and vaccine safety and risk communication guidelines.
- Revising, designing, printing, and distributing 30,000 reporting tools.
- Conducting supportive supervision visits to more than 700 active surveillance and passive reporting vaccination sites.
- Organizing intra-action review on COVID-19 vaccine supply management and pharmacovigilance with the Ministry of Health, RHBs, EFDA, and relevant partners, including GAVI the Vaccine Alliance.
- Organizing AEFI training and orientation for about 1,500 regulatory experts and healthcare providers from vaccination sites.
- Supporting the government in conducting three successful rounds of COVID-19 vaccination campaigns to increase coverage.
By April 2022, more than 38,000 vaccinated individuals were on active surveillance, with data collected for all four COVID-19 vaccines being administered. More than 29,000 reports were collected through active surveillance and passive reporting. About 9,700 reports were entered into the global WHO database, of which 75 were claimed to be serious and 30 to be severe. Investigations were conducted on 48 cases and, out of these, causality assessments were conducted to 29 AEFI cases. Three casualty cases were deemed vaccine product-related reactions, and the regulatory authority has written its assessments with recommendations to the relevant unit of the Ministry.
In its assessments, EFDA has recommended to the Ministry that people should be screened for COVID-19-related symptoms—which can be a risk factor for adverse events—and to have adrenaline available to manage serious reactions.
To adapt this surveillance program to other countries, GHSC-PSM recommended some best practices to follow:
- Prioritize training, site-level supportive supervision, close follow-up, and collaboration and coordination with public health programs and regulators.
- Widen adverse drug event reporting methods to include e-reporting and mobile apps.
- Implement active surveillance.
- Organize intra-action reviews to assess challenges, best practices, and next steps with relevant stakeholders to strengthen monitoring and evaluation.
- All these lessons and experiences on implementing and conducting safety surveillance of COVID-19 vaccines are shared on a platform that has brought together Ethiopia, Ghana, Nigeria, and South Africa through the African Union’s Smart Safety Surveillance (AU-3S) program.